Congenital Heart Disease: Cases
Congenital Heart Disease: Cases
Pediatric Emergency Playbook
pemplaybook.org
info_outline Congenital Heart Disease: Plumbing & Air for the Emergency Physician
Congenital Heart Disease: Plumbing & Air for the Emergency Physician
Pediatric Emergency Playbook
pemplaybook.org
info_outline Precipitous Delivery
Precipitous Delivery
Pediatric Emergency Playbook
info_outline From the Ashes of SIRS: The Phoenix Sepsis Score
From the Ashes of SIRS: The Phoenix Sepsis Score
Pediatric Emergency Playbook
pemplaybook.org
info_outline Torticollis
Torticollis
Pediatric Emergency Playbook
www.PEMplaybook.org
info_outline Resuscitative Umbilical Vein Catheterization
Resuscitative Umbilical Vein Catheterization
Pediatric Emergency Playbook
pemplaybook.org
info_outline Update 2023
Update 2023
Pediatric Emergency Playbook
pemplaybook.org
info_outline Neonatal Resuscitation
Neonatal Resuscitation
Pediatric Emergency Playbook
pemplaybook.org
info_outline Stridor, Stertor, and Noisy Breathing
Stridor, Stertor, and Noisy Breathing
Pediatric Emergency Playbook
PEMplaybook.org
info_outline Brief, Huddle, and Debrief in the PED
Brief, Huddle, and Debrief in the PED
Pediatric Emergency Playbook
info_outline
It's a busy shift. Today no one seems to have a chief complaint.
Someone sends a troponin on a child. Good, bad, or ugly, how are you going to interpret the result?
And while we’re at it – what labs do I need to be careful with in children – sometimes the normal ranges of common labs can have our heads spinning!
Read on to go from bread-and-butter pediatric blood work to answer the question – what’s up with troponin, lactate, d-dimer, and BNP in kids?
A fundamental tenet of emergency medicine:
We balance our obligation to detect a dangerous condition with our suspicion of the disease in given patient.
Someone with a cough and fever may simply have a viral illness, or he may have pneumonia. Our obligation is to evaluate for the pneumonia. It’s ok if we “miss” the diagnosis of a cold. It could be bad if we don’t recognize the pneumonia.
How do we decide? Another fundamental concept:
The threshold.
Depending on the disease and the particular patient, we have a threshold for testing, and the threshold for treating. Every presentation – and every patient for that matter – has a complicated interplay between what we are expected to diagnose, how much we suspect that particular serious diagnosis, and where testing and treating come into play.
What's wrong with "throwing on some labs"?
Easy to do right? They are but a click away…
Often a good history and physical exam will help you to calibrate your investigational thresholds. This is especially true in children – the majority of pediatric ambulatory visits do not require blood work to make a decision about acute care. If your patient is ill, then by all means; otherwise, consider digging a bit deeper into the history, get collateral information, and make good use of your general observation skills.
First, a brief word about basic labs.
The punchline is, use a pediatric reference.
If you don’t have a trusted online reference available during your shift, make sure you have something like a Harriett Lane Handbook accessible to you. Don’t rely on your hospital’s lab slip or electronic medical record to save you, unless you are sure that they use age-specific pediatric reference ranges to flag abnormal values. Believe it or not, in this 21st century of ours, some shops still use adult reference ranges when reporting laboratory values on children.
Notable differences in basic chemistries
Potassium: tends to run a bit higher in infants, because for the first year of life, your kidneys are inefficient in excreting potassium.
BUN and creatinine: lower in children due to less muscle mass, and therefore less turnover (and usually lack of other chronic disease)
Glucose: tends to run lower, as children are hypermetabolic and need regular feeding (!)
Alkaline phosphatase: is always high in normal, growing children, due to bone turn over (also fond in liver, placenta, kidneys)
Ammonia: high in infancy, due to immature liver, trends down to normal levels by toddlerhood
ESR and CRP: low in healthy children, as chronic inflamation from comorbidities is not present; both increase steadily with age
Thyroid function tests: all are markedly high in childhood, not as a sign of disease, but a marker of their increased metabolic activity
Big Labs
Troponin
Reliably elevated in myocarditis, and may help to distinguish this from pericarditis (in addition to echocardiography)
Other causes of elevated troponin in children include: strenuous activity, status epilepticus, toxins, sepsis, myocardial infarction (in children with congenital anomalies). Less common causes of troponemia are: Kawasaki disease, pediatric stroke, or neuromuscular disease.
Don't go looking, if you won't do anything with the test.
Brain natriuretic peptide (BNP)
In adults, we typically think of a BNP < 100 pg/mL as not consistent with symptoms caused by volume overload.
Luckily, we have data in children with congenital heart disease as well. Although each company's assay reports slightly different cut-offs, in general healthy pediatric values match healthy adult values.
One exception is in the first week of life, when it is high even in healthy newborns, due to the recent transition from fetal to newborn circulation.
Use of BNP in children has been studied in both clinic and ED settings. Cohen et al. in Pediatrics used BNP to differentiate acute heart failure from respiratory disease in infants admitted for respiratory distress. They compared infants with known CHF, lung disease, and matched them with controls.
Later, Maher et al. used BNP in the emergency department to differentiate heart failure from respiratory causes in infants and children with heart failure and those with no past medical history.
The bottom line is:
BNP reliably distinguishes cardiac from respiratory causes of shortness of breath in children with a known diagnosis of heart failure.
D-dimer
To cut to the chase: d-dimer for use as a rule-out for pulmonary embolism has not been studied in children.
The only data we have in using d-dimer in children is to prognosticate in established cases. It is only helpful to track therapy for children who have chronic clots.
This is where our adult approach can get us into trouble. Basically, think of the d-dimer in children like it doesn’t even exist. It’s not helpful in our setting for our indications. An adult may have an idiopathic PE – in fact, up to a third of adults with PE have no known risk factor, which makes decision tools and risk stratification important in this population.
Children with PE almost always have a reason for it.
There is at least one identifiable risk factor in up to 98% of children with pulmonary embolism. The majority have at least two risk factors.
If you’re suspecting deep venous thrombosis, perform ultrasonography, and skip the d-dimer.
If you’re worried about PE, go directly to imaging. In stable patients, you may elect to use MR angiography or VQ scan, but most of us will go right to CT angiography. Radiation is always a concern, but if you need to know, get the test.
This is yet another reminder that your threshold is going to be different in children when you think about PE – they should have a reason for it. After you have excluded other causes of their symptoms, if they have risk factors, and you are still concerned, then do the test you feel you need to keep this child safe.
You are the test.
Risk factors only inform you, and you’ll have to just pull the trigger on testing in the symptomatic child with risk factors.
Lactate
A sick child with sepsis syndrome?
The short answer – yes.
In the adult literature, we know that a lactate level above 4 mmol/L in patients with severe sepsis was associated with the need for critical care. This has been studied in children as well, and an elevated lactate in children – typically above 4 – was a predictor of prolonged ICU course and mortality in septic patients.
The acute recognition and treatment of sepsis is first and foremost, clinical.
And it’s all about perfusion and providing oxygen to the tissues. Lactate and other laboratory testing is not a substitute for clinical assessment – it should be used as an extension of your assessment. There are two main reasons for an elevated lactate: the stress state and the shock state.
The stress state is due to hypermetabolism and an increase in glycolysis, as an example, in early sepsis. The shock state is due to tissue hypoxia, seen in septic shock. The confusion and frustration with lactate is that we often test the wrong people for it.
We could use it to track treatment, and see if we can clear the lactate; decreased lactate levels are associated with a better outcome in adults. Serial clinical assessments are even more useful to gauge your success with treatment.
We should use lactate to detect occult shock. Children compensate so well for shock, that subtle tissue hypoxia may not be detected until later. It may inform your decision for level of care, intensive care versus some other lower level.
Have you every been in this situation:
"Why, oh why, did we send a lactate?"
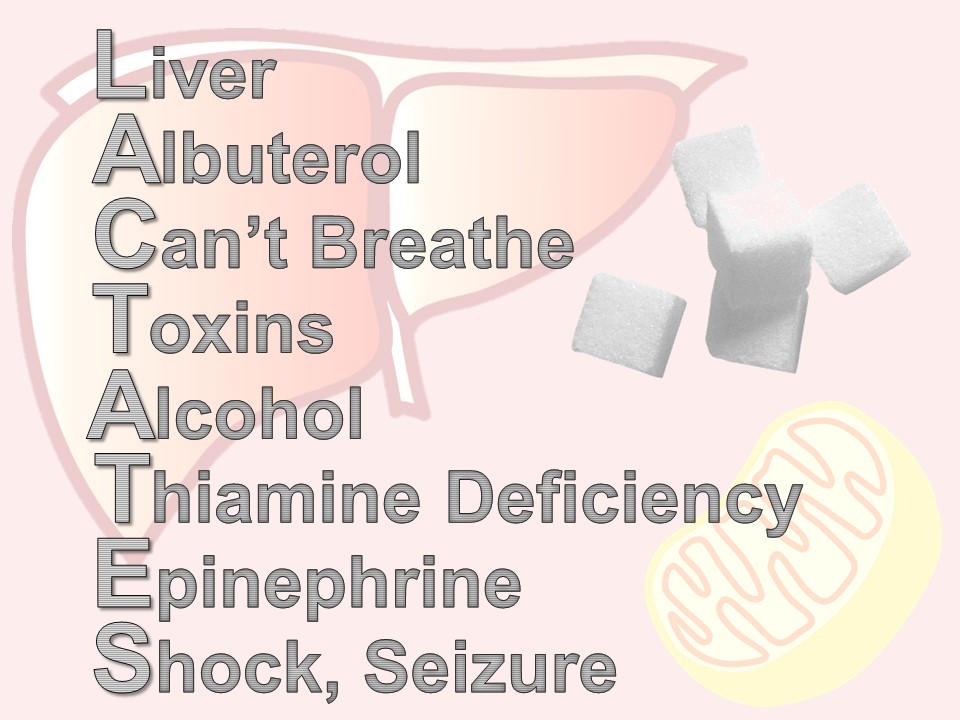
There are times when a lactate is ordered – maybe by protocol or maybe accidentally – or maybe in retrospect, the patient didn’t need it. Here is a quick mnemonic to remember the reasons for an elevated lactate: LACTATES
L – liver – any liver disease affects how lactate is metabolized by the Cori cycle
A – albuterol (or for our international friends, salbutamol), beta-agonists like albuterol, increase lactate production via cyclic amp
C – “can’t breathe” – respiratory distress and increased work of breathing shifts the ratio of aerobic and anerobic repiration
T – toxins – all kinds of wonder drugs and recreational drugs do it – look up your patient’s list if you’re suspicious
A – alcohol, not an infrequent offender
T – thiamine deficiency – think of this in your cachectic or malnourished patients
E – epinephrine – a by-product of the cori cycle, how lactate is metabolized. Difficult to interpret lactates when a patient is on an epinephrine drip.
S – seizure or shock – most commonly septic, but can be any type: cardiogenic, bstructive, hypovolemic, distributive.
Bottom line: high serum lactate levels have been associated with morbidity and mortality in children with sepsis and trauma, the two best-studied populations.
A summary of how labs can help you – or hurt you – in pediatric emergency medicine:
- Have a good reference for normal values and always be skeptical of how your lab reports them.
- Troponin testing is great for the child with suspected cardiogenic shock, myocarditis, or in unwell children with congenital heart disease.
- BNP in children can be used just like you do in adults – to get a sense of whether the presenting symptoms are consistent with heart failure.
- D-dimer is mostly a waste of time in the PED.
- Lactate can be useful in the right patient – use it to risk-stratify the major trauma patient or the patient with sepsis that may be suffering from occult shock.
- And lastly, make sure that you are mindful of your threshold for testing, and our threshold for treatment. If will vary by disease and by the patient at hand.
References
Troponin
Gupta SK, Naheed Z. Chest Pain in Two Athletic Male Adolescents Mimicking Myocardial Infarction. Pediatr Emer Care. 2014;30: 493-495.
Kelley WE, Januzzi JL, Christenson RH. Increases of Cardiac Troponin in Conditions other than Acute Coronary Syndrome and Heart Failure. Clinical Chemistry. 2009; (55) 12:2098–2112.
Kobayashi D, Aggarwal S, Kheiwa A, Shah N. Myopericarditis in Children: Elevated Troponin I Level Does Not Predict Outcome. Pediatr Cardiol. 2012; 33:1040–1045.
Koerbin G, Potter JM, Abhayaratna WP et al. The distribution of cardiac troponin I in a population of healthy children: Lessons for adults. Clinica Chimica Acta. 2016; 417: 54–56.
Liesemer K, Casper TC, Korgenski K, Menon SC. Use and Misuse of Serum Troponin Assays in Pediatric Practice. Am J Cardiol. 2012;110:284 –289.
Newby KL et al. for the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. ACCF 2012 Expert Consensus Document on Practical Clinical Considerations in the Interpretation of Troponin Elevations. J Am Coll Cardiol. 2012; 60(23): 2427-2463.
Schwartz MC, Wellen S, Rome JJ et al. Chest pain with elevated troponin assay in adolescents. Cardiology in the Young; 2013. 23: 353–360.
BNP
Auerbach SR, Richmond ME, Lamour JM. BNP Levels Predict Outcome in Pediatric Heart Failure Patients Post Hoc Analysis of the Pediatric Carvedilol Trial. Circ Heart Fail. 2010;3:606-611.
Cohen S, Springer C, Avital A et al. Amino-Terminal Pro-Brain-Type Natriuretic Peptide: Heart or Lung Disease in Pediatric Respiratory Distress? Pediatrics. 2005;115:1347–1350.
Fried I, Bar-Oz B, Algur N et al. Comparison of N-terminal Pro-B-Type Natriuretic Peptide Levels in Critically Ill Children With Sepsis Versus Acute Left Ventricular Dysfunction. Pediatrics. 2006; 118(4): 1165-1168.
Koch A, Singer H. Normal values of B type natriuretic peptide in infants, children, and adolescents. Heart. 2003;89:875–878.
Maher KO, Reed H, Cuadrado A et al. , B-Type Natriuretic Peptide in the Emergency Diagnosis of Critical Heart Disease in Children. Pediatrics. 2008;121:e1484–e1488.
Mir TS, Marohn S, Laeer S, Eistelt M. Plasma Concentrations of N-Terminal Pro-Brain Natriuretic Peptide in Control Children From the Neonatal to Adolescent Period and in Children With Congestive Heart Failure. Pediatrics. 2002;110(6)1:6.
Mir TS, Laux R, Hellwege HH et al. Plasma Concentrations of Aminoterminal Pro Atrial Natriuretic Peptide and Aminoterminal Pro Brain Natriuretic Peptide in Healthy Neonates: Marked and Rapid Increase After Birth. Pediatrics. 2003;112:896–899.
D-Dimer
Goldenberg NA, Knapp-Clevenger RA, Manco-Johnson MJ. Elevated Plasma Factor VIII and d-Dimer Levels as Predictors of Poor Outcomes of Thrombosis in Children for the Mountain States Regional Thrombophilia Group. Pediatrics. 2003;112:896–899.
Manco-Johnson MJ. How I treat venous thrombosis in children. Blood. 2006; 107(1)21-31.
Naqvi M, Miller P, Feldman L, Shore BJ. Pediatric orthopaedic lower extremity trauma and venous thromboembolism. J Child Orthop. 015;9:381–384.
Parasuraman S, Goldhaber SZ. Venous Thromboembolism in Children. Circulation. 2006;113:e12-e16.
Strouse JJ, Tamma P, Kickler TS et al. D-Dimer for the Diagnosis of Venous Thromboembolism in Children. N Engl J Med. 2004;351:1081-8.
Lactate
Andersen LW, Mackenhauer J, Roberts JC et al. Etiology and therapeutic approach to elevated lactate. Mayo Clin Proc. 2013; 88(10): 1127–1140.
Bai et al. Effectiveness of predicting in-hospital mortality in critically ill children by assessing blood lactate levels at admission. BMC Pediatrics. 2014; 14:83.
Scott HF, Donoghue AJ, Gaieski DF et al. The Utility of Early Lactate Testing in Undifferentiated Pediatric Systemic Inflammatory Response Syndrome. Acad Emerg Med. 2012; 19:1276–1280.
Shah A, Guyette F, Suffoletto B et al. Diagnostic Accuracy of a Single Point-of-Care Prehospital Serum Lactate for Predicting Outcomes in Pediatric Trauma Patients. Pediatr Emer Care. 2013; 29:715-719.
Topjian AA, Clark AE, Casper TC et al. for the Pediatric Emergency Care Applied Research Network. Early Lactate Elevations Following Resuscitation From Pediatric Cardiac Arrest Are Associated With Increased Mortality. Pediatr Crit Care Med. 2013; 14(8): e380–e387.
This post and podcast are dedicated to Daniel Cabrera, MD for his vision and his leadership in thinking 'outside the box'.
Troponin | BNP | D-Dimer | Lactate
Powered by #FOAMed -- Tim Horeczko, MD, MSCR, FACEP, FAAP