Congenital Heart Disease: Cases
Congenital Heart Disease: Cases
Pediatric Emergency Playbook
pemplaybook.org
info_outline Congenital Heart Disease: Plumbing & Air for the Emergency Physician
Congenital Heart Disease: Plumbing & Air for the Emergency Physician
Pediatric Emergency Playbook
pemplaybook.org
info_outline Precipitous Delivery
Precipitous Delivery
Pediatric Emergency Playbook
info_outline From the Ashes of SIRS: The Phoenix Sepsis Score
From the Ashes of SIRS: The Phoenix Sepsis Score
Pediatric Emergency Playbook
pemplaybook.org
info_outline Torticollis
Torticollis
Pediatric Emergency Playbook
www.PEMplaybook.org
info_outline Resuscitative Umbilical Vein Catheterization
Resuscitative Umbilical Vein Catheterization
Pediatric Emergency Playbook
pemplaybook.org
info_outline Update 2023
Update 2023
Pediatric Emergency Playbook
pemplaybook.org
info_outline Neonatal Resuscitation
Neonatal Resuscitation
Pediatric Emergency Playbook
pemplaybook.org
info_outline Stridor, Stertor, and Noisy Breathing
Stridor, Stertor, and Noisy Breathing
Pediatric Emergency Playbook
PEMplaybook.org
info_outline Brief, Huddle, and Debrief in the PED
Brief, Huddle, and Debrief in the PED
Pediatric Emergency Playbook
info_outline
Seemingly vague, but potentially dangerous...
common, but possibly with consequences...
...or maybe just plain frustrating.
Let's talk risk stratification, diagnosis, and management.
Primary or Secondary?
We can make headache as easy or as complicated as we like, but let's break it down to what we need to know now, and what the parents need to know when they go home.
Primary headaches: headaches with no sinister secondary cause – like tension or migraine – are of course diagnoses of exclusion (cluster headache is exceedingly rare in children).
Secondary headaches: headaches due to some underlying cause -- are what we need to focus on first.
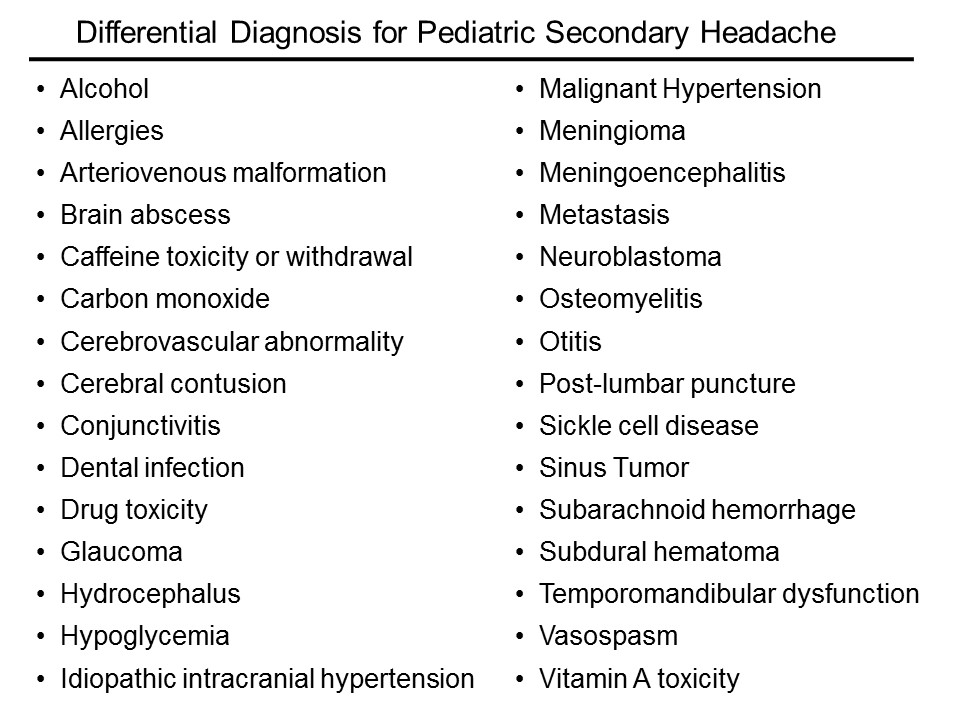
The list of etiologies is vast; here is just a sampling:
How do I sort this out?
Ask yourself three main questions:
Is it a tumor?
Is it an infection?
Is it a bleed?
Is it a tumor?
Some historical features are high-yield in screening for signs or symptoms consistent with a space occupying lesion.
Progression and worsening of symptoms over time
Associated vomiting
Pain only in the occiput
Headache that is worse with Valsalva – ask if coughing, urinating, or defecating affects the headache
Does this headache wake the child from sleep?
Is it worse in the morning just after getting up?
Conversely, the absence of some historical features may increase suspicion of a space-occupying lesion
No family history of migraine
No associated aura with the headache.
Who needs neuroimaging?
The short answer is, if the child has an abnormal exam finding, then obtain a non-contrast head CT in the ED. If you’re worried enough to get imaging, then you should not feel great about sending him to an expedition to MRI.
The reassuring point is that for a child with a normal neuro exam, we have time to figure this out. For the recurrent headache, outpatient MRI really is the way to go if at all possible – not only do we forgo unnecessary radiation, but MRI is more likely to reveal the cause – or rule out the concern.
Medina et al. in Pediatrics reported on children with headache suspected of having a brain tumor. They stratified patients into low, intermediate, and high risk, based on clinical predictors from the history and physical. All had imaging. They then calculated probability of tumor in each group.
The low risk group had a 0.01% probability of tumor. The intermediate group 0.4%, and the high-risk group had only a 4% probability of tumor. The take-home message is that in the stable patient with a normal neurologic exam and no red flags, time is on our side.
The American Academy of Neurology's most recent guidelines, published first in 1994 and revised in 2004.
1. Neuroimaging on a routine basis is not indicated with recurrent headaches and a normal neurologic exam
2. Neuroimaging should be considered in children with an abnormal exam.
3. Neuroimaging should be considered in children with recent onset of severe headache, change in the type of headache, or associated features that suggest neurologic dysfunction
Is it an infection?
This is nothing new: if you think you need to perform a lumbar puncture, then you’re right. Go after the diagnosis when it meets your threshold for testing.
The difficulty is in the child who just has a headache, plus or minus symptoms that may be viral syndrome.
Dr Curtis et al. in Pediatrics did a systematic review of Clinical Features Suggestive of Meningitis in Children. In the history, only obvious features were helpful in this study: bulging fontanel in the infant or neck stiffness in the older child. Both increased the likelihood of meningitis by 8-fold.
In the physical examination, the only reliable predictors in this study were poor general appearance or a change in behavior.
You will catch those cases, because you would have tuned into meningitis early on -- especially in the unvaccinated.
What about all-comers with fever and headache? The presence of a high fever (so greater than 40 °C) only conferred a positive likelihood ratio of 2.9, only marginally predictive. Reassuring is that for temperatures less than 40 °C, the LR was 1 for meningitis.
In other words, a fever less than 40 °C was just as likely to be present with or without meningitis.
Is it a bleed?
Does this child have some underlying disorder? For example, sickle cell disease, hypertension, rheumatologic disease, or some other endocrine or metabolic disease, such as a mitochondrial disorder?
In chronically ill children, consider cerebral sinus venous thrombosis, vasculitis, ischemia, or hemorrhage.
Arteriovenous malformation (AVM) is the hemorrhage we fear the most.
We really don’t know enough about arteriovenous malformations in the brain to say what is the typical presentation. They may be completely asymptomatic, until they rupture. Even the headache presentation is variable.
Think, headache PLUS.
New headache plus…vomiting.
Headache plus…it’s unilateral and new for the patient.
Headache plus…a new seizure.
Headache plus…focal neuro deficits, that may be transient, due to a vascular steal phenomenon.
Two illustrative cases of arteriovenous malformation:
1. An eleven-year-old girl presents to the ED with new headache, nausea, and vomting in the morning, then had a generalized seizure later that day, and presents with a low GCS. She was intubated, CT confirmed the AVM. She had a right frontal intraparenchymal bleed with midline shift. She underwent clot evacuation and extirpation of the intertwined arteries and veins.
2. A nine-year old girl presented to the ED with headache for two days, constant, then one day of nausea and vomiting. On presentation, she was altered, and had slow-reacting pupils. She also underwent evacuation, and only on histopathology did they find a single, arterialized vein.
Primary Headache: Presumptive Impression
Tension headaches are the most common in children and adults. As in adults, the tension headache is band-like, pressure, tighetening, and often associated with muscle aches in the neck and shoulders.
Find out how often they occur, and whether there is any pattern of worsening symptoms, or if the symptoms seem to be related to sleep hygiene, video games, too much digital screen time. Also, screen for lack of exercise, poor diet, stress, and all of the other good questions you usually ask.
Treat the cause or counsel about lifestyle modification, and offer PO hydration and an NSAID, like ibuprofen or acetaminophen (paracetamol).
Non-pharmacologic techniques like heat packs, rest, stress relief, and a little TLC always help. Be careful not to encourage overreacting to the headache – sometimes we see a pattern of headache, attention, and more headache that can take root. Also look for overuse of medications, which may be the culprit in up to 50% of chronic headaches. Taking NSAIDs 3 or more times per week is associated with medication-induced headache, or cephalalgia medicamentosa.
We often fail to identify migraine headaches in children in the ED, likely for two reasons: prevalence of migraine increases with age, and children don’t present exactly like adults.
Stewart et al. in Neurology, report a prevalence of migraine in children that increases with age: 3 to 7 years of age was 2%; 7 to 11 years of age, 7%; and 11 to 20 years of age, 20%
Pearl: migraines are most commonly bilateral and temporal in children. They resemble "adult" tension headaches, but are much more severe.
We may not be able to sort this out in the ED. The point here is that migraines in children are more common that we may expect, and they can interfere with school performance, with social development, or even with family dynamics and overall stress burden.
Primary Headache Diagnosis: Not (Usually) "Our Thing"
You noticed that we treated before we knew exactly the etiology; such is Emergency Medicine.
We may not be able to make a specific, definitive primary headache diagnosis in the ED, but we should be aware of the criteria to help counsel patients and families.
Tension headache is the most common, but it requires multiple, similar episodes: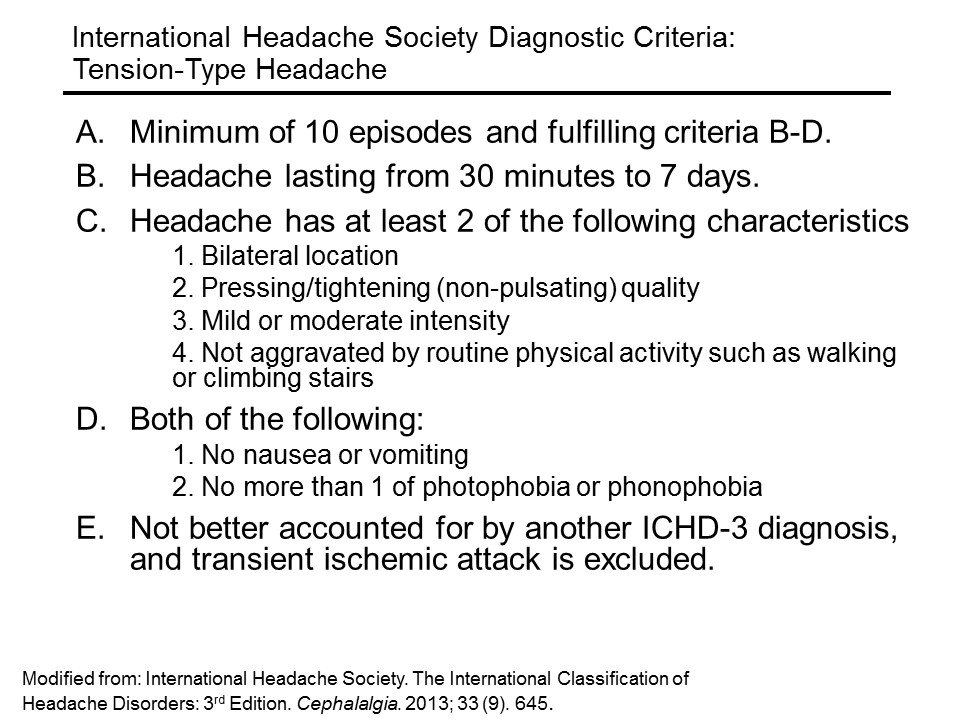
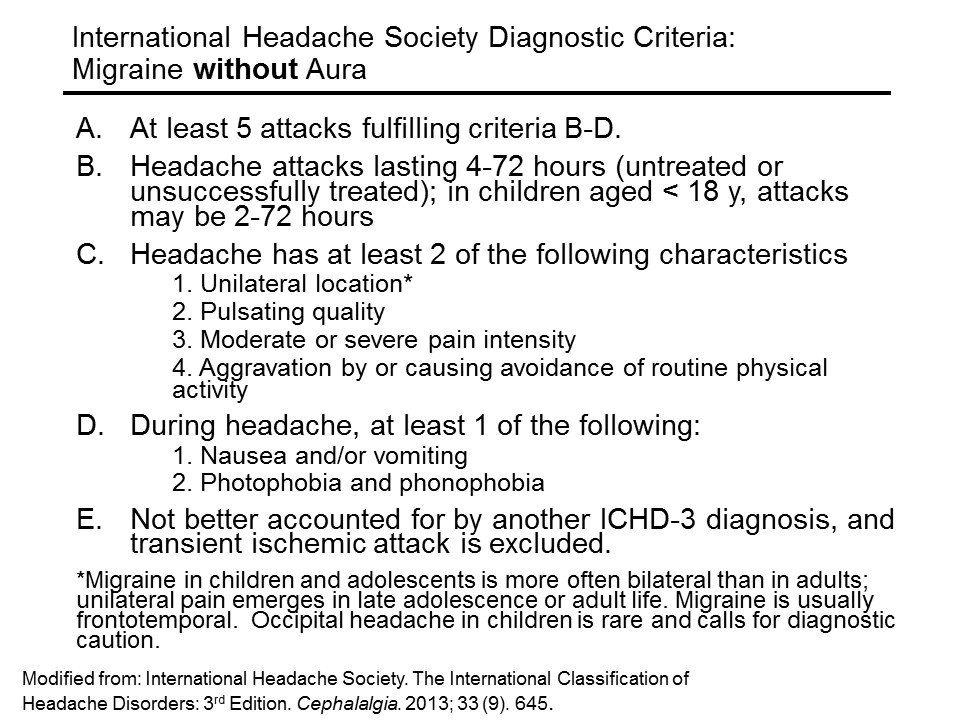
Migraine headache (without aura) requires less episodes, but more specific features:
An aura is a fast-pass to diagnosis of migraine: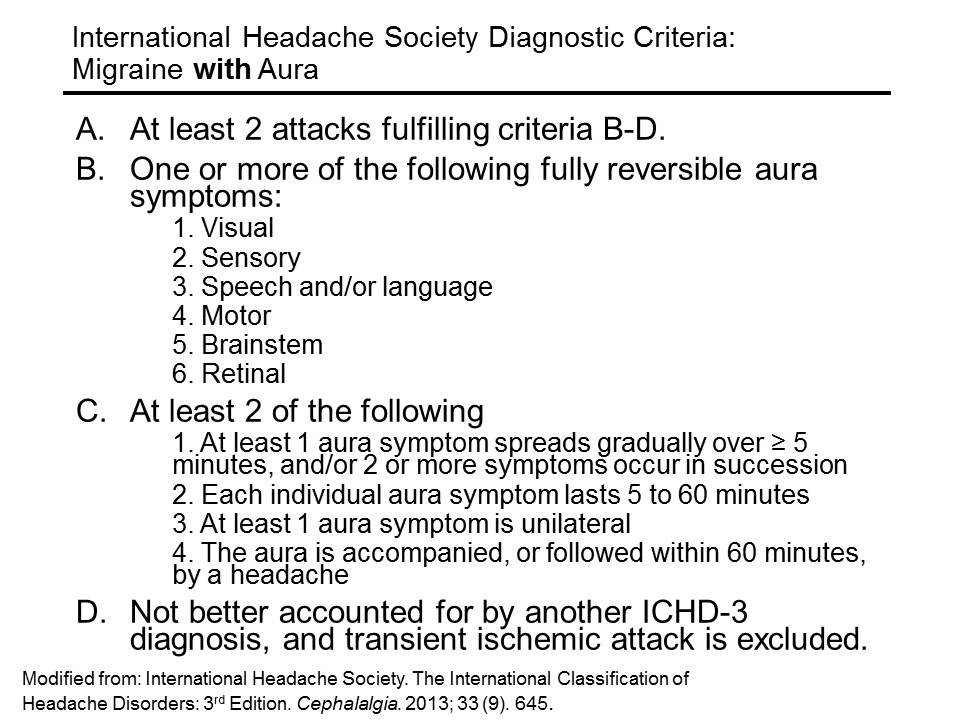
Primary Headache Management
So how do we treat primary headaches? If you feel this is a mild tension headache, fluids by mouth and a simple NSAID are probably all that is needed, in addition to a heaping dose of reassurance. Ibuprofen (10 mg/kg/dose q 6h, up to 600 mg) for a short course has the most evidence basis. Acetaminophen (paracetamol) (15 mg/kg/dose q6 h) for a short course may also be given.
Abortive treatments with the triptans may have been tried at home, but if they are coming to see us, we are past the point where triptans will be helpful.
For the primary headache that is resistant to NSAIDs, IV therapy may be considered.
If you’re going for IV, a nice evidence-based migraine cocktail is the following:
1. A bolus of 20 ml/kg of normal saline, up to a liter
2. Ketorolac (0.5 mg/kg; max, 30 mg)
3. Diphenhydramine (2 mg/kg; max, 50 mg)
4. Prochlorperazine (0.1 mg/kg; max, 10 mg)
Dr Kaar et al. in Pediatric Emergency Care evaluated the safety and efficacy of their institution’s standardized pediatric migraine practice guideline in the emergency department, which used ths cocktail, based on the best evidence available. In their retrospective chart review, they found the average visual pain scale drop from 7.8 to 2.1
There were no adverse events reported.
So, really you can treat children with migraines very similarly to adults.
Other treatments on the horizon (still under investigation) in children include IV adjuncts such as magnesium, valproic acid, and dexamethasone.
Aftercare and Recurrence Prevention
For everyone who is going home, take just a moment to talk about the importance of sleeping well, eating well, getting exercise, limiting digital screen time, and trying to improve ways of dealing with stress.
When all else fails, and the parent has “heard it all”: get them started on a headache diary.
Take a piece of paper, fold it in half, and start a template for them to work on in a spiral notebook. Start a sample entry for them, with the date and time the headache started, what it felt like, what was happening just before, what made the headache better, any dose of medications given, how long it lasted, and what the patient did after. There are even free apps that will track the headache pattern.
This is the first thing a neurologist will start them on – and it’s sometimes a selling point to the parent that the time spent waiting for a referral to a neurologist is not waste – they will actually be in better shape and can move things along faster. It also gives them some sens of control of what can be a draining situation.
Summary and Mental Road Map
If you were thinking meningitis or acute bleed, especially with fever or meningismus, get a CT first if you see signs of increased intracranial pressure, or if there is an abnormal neuro exam. Otherwise go straight to the lumbar puncture (LP).
In the afebrile child with a normal exam, give symptomatic relief, briefly counsel them, and arrange for follow-up.
In the afebrile child with an abnormal exam, obtain a CT in the ED. If negative, either admit for MRI if you are still concerned, or consider LP for idiopathic intracranial hypertension (pseudotumor cerebri).
Talk with parents early about expectations, and offer them some friendly advice on prevention. Refer patients to the primary care provider or neurologist if the presentation is more involved.
After a good history and physical examination in the ED that results in no red flags, we have time on our side. Help the family through the process by explaining the next steps and what can be done in the meantime. Compassion and a plan: sometimes these are our most powerful allies.
References
This post and podcast are dedicated to Mark Wilson, PhD, BSc, MBBChir, FRCS(SN), MRCA, FIMC, FRGS for his #FOAMed generosity, candor, humility, and dedication to the care of the acutely ill and injured. Thank you.
Powered by #FOAMed -- Tim Horeczko, MD, MSCR, FACEP, FAAP