 Fix Shoulder External Rotation FAST (& for Good)
Fix Shoulder External Rotation FAST (& for Good)
The Zac Cupples Show
🏃 Tired of searching for how to move better on youtube? Get personalized coaching with myself and my coaches: 🚀 Unlock Your Shoulder Mobility! 🚀 🔥 Struggling with stiff, tight shoulders that ruin your high-fives and throwing game? Dive into our latest video where I'll guide you through groundbreaking exercises designed to supercharge your shoulder mobility! 🏋️♂️ 🤩 Witness firsthand how to improve ribcage mobility, crucial for optimal shoulder function. Start with a simple move using a yoga block to enhance your shoulder external rotation, making daily activities...
info_outline 20 Second Tight Psoas Release (& Fix Long-Term)
20 Second Tight Psoas Release (& Fix Long-Term)
The Zac Cupples Show
🏃 Tired of searching for how to move better on youtube? Get personalized coaching with myself and my coaches: 🚀 Unlock Hip Flexor Freedom in Seconds! 🚀 Discover the secret to banishing hip flexor tightness with lightning speed! Dive into a game-changing routine that promises to transform your mobility and comfort in under a minute. Say goodbye to discomfort and hello to effortless movement. You'll have the chillest psoas in da game! #psoas #HipFlexor #posture #pain #mobility ⏰ TIMESTAMPS ⏰ (00:00) - This release WORKS (01:07) - How long does it last though? (the long...
info_outline Fix Rib Flare FAST (In Less Than 5 Minutes a Day)
Fix Rib Flare FAST (In Less Than 5 Minutes a Day)
The Zac Cupples Show
🏃 Tired of searching for how to move better on youtube? Get personalized coaching with myself and my coaches: 🌟 **Transform Your Posture: The Ultimate Rib Flare Fix!** 🌟 Dive into a groundbreaking journey to reshape your ribcage and enhance your mobility. Discover three pivotal exercises designed to address the common yet overlooked issue of rib flare, transforming not just your posture but your overall movement quality. **Embark on your transformation journey now!** #RibFlare #Posture #Mobility (00:00) - Can this even be fixed? (00:41) - This MASSIVE mistake ruins your results...
info_outline 3 Exercises That Fix 90% of Problems
3 Exercises That Fix 90% of Problems
The Zac Cupples Show
🏃 Tired of searching for how to move better on youtube? Get personalized coaching with myself and my coaches: 🌟 Unlock Ultimate Mobility: A Game-Changer for Pain-Free Movement! 🌟 Embark on a transformative journey to conquer common mobility restrictions with three groundbreaking exercises. Dive into a world where enhanced flexibility, strength, and performance are within your grasp. **Experience the revolution in mobility today!** #Mobility #PainFreeLiving #Flexibility ⏰ TIMESTAMPS ⏰ (00:00) - Rotation nation (01:33) - The reason movement becomes limited (03:49) - How...
info_outline Fix Pooch Belly Fast (In Less Than 5 Minutes a Day)
Fix Pooch Belly Fast (In Less Than 5 Minutes a Day)
The Zac Cupples Show
🏃 Tired of searching for how to move better on youtube? Get personalized coaching with myself and my coaches: 🌟 **Unlock the Secret to a Flatter Belly - No Crunches Required!** 🌟 Discover groundbreaking exercises that defy traditional fat loss and posture correction methods. Dive into a revolutionary approach that reshapes your abdominal appearance by addressing the underlying postural components. Say goodbye to the pooch belly with simple, effective moves that promise visible changes. **Embark on your journey to a sleeker silhouette today!** #FlatterBelly #PostureCorrection...
info_outline How To Improve Sitting (It's Not JUST Posture)
How To Improve Sitting (It's Not JUST Posture)
The Zac Cupples Show
🏃 Care about improving your health, mobility, and fitness? Work with myself or one of my coaches. Schedule here: 🌟 **Transform Your Sitting Experience!** 🌟 Unlock the secret to comfortable sitting with groundbreaking strategies that defy conventional wisdom. From eye-saving techniques to posture-transforming exercises, this video is your ultimate guide to conquering discomfort in the digital age. Say goodbye to soreness and hello to a new era of ergonomic enlightenment. **Dive in and revolutionize the way you sit today!** #SittingComfort #Ergonomics #sitting #HealthyPosture...
info_outline Fix Posture and Muscle Imbalances FAST
Fix Posture and Muscle Imbalances FAST
The Zac Cupples Show
🏃 Care about improving your health, mobility, and fitness? Work with myself or one of my coaches. Schedule here: 🌟 Unlock Symmetry: Break Free from Imbalance and Posture Myths 🌟 Feeling off-kilter, twisted, or battling muscle imbalances? It's time to challenge the conventional stretch-and-strengthen approach and explore the truth behind achieving a more balanced body. This video is your guide to debunking myths and embracing the nuances of your unique posture. What You'll Discover: - Insight into why striving for perfect symmetry might not be the goal. - The critical role of the...
info_outline Fix Your Shoulder Internal Rotation FAST
Fix Your Shoulder Internal Rotation FAST
The Zac Cupples Show
🏃 Care about improving your health, mobility, and fitness? Work with myself or one of my coaches. Schedule here: 🌟 Transform Your Shoulder Mobility: The Ultimate Guide 🌟 Struggling with limited shoulder internal rotation? Discover the game-changing exercise that's revolutionizing shoulder health and performance. This video is your roadmap to unlocking the full potential of your shoulders, ensuring you can reach, lift, and perform without pain. What You'll Learn: - The critical role of the rib cage in achieving optimal shoulder rotation. - A step-by-step guide to exercises that...
info_outline You Won't Believe What This Does for Your Neck
You Won't Believe What This Does for Your Neck
The Zac Cupples Show
🏃 Care about improving your health, mobility, and fitness? Work with myself or one of my coaches. Schedule here: 🌟 Unlock Neck Comfort: Overlooked Solutions for Persistent Pain 🌟 Tired of neck pain that just won't quit, even after stretching, chin tucks, and posture adjustments? This video is your key to unlocking the relief you've been searching for. What You'll Discover: - Innovative strategies to address often overlooked factors contributing to neck discomfort. - A transformative exercise targeting the thoracic spine, the true base of your neck, for immediate relief. -...
info_outline 3 Exercises That Fix 90% of Low Back Pain
3 Exercises That Fix 90% of Low Back Pain
The Zac Cupples Show
🏃 Care about improving your health, mobility, and fitness? Work with myself or one of my coaches. Schedule here: 🌟 Transform Your Lower Back Comfort with Just 3 Moves! 🌟 Battling lower back discomfort? It's time to revolutionize your approach to back health with three essential movements designed to enhance mobility and alleviate pain. What's Inside: - Discover three foundational movements to address common lower back mobility needs. - Learn techniques to distribute spinal load more evenly, ensuring each segment moves optimally. - Master the art of creating more space in your...
info_outlineHow a dentist can improve your sleep, breathing, and more
If you have perfect sleep, NEVER mouth breathe, and have excellent tongue posture, then you can skip this post.
But if you are like the rest of us, no doubt you or your clients struggle in one or many of these areas.
What if all of these issues were related to the structure of your mouth?
That’s why I interviewed Dr. Brian Hockel, a dentist who I work with personally, and a leading expert in the field of dentistry and airway orthodontics.
[caption id="attachment_12956" align="aligncenter" width="600"] The legend![/caption]
The legend![/caption]
In this podcast, you’ll learn:
- How facial structure can impact breathing and tongue position
- Why a CPAP doesn’t really fix sleep apnea
- How a well-trained dentist can improve mouth position to enhance your sleep and breathing
- How occlusion, tooth contact, may not be the exact science that people make it out to be
- What you need to look for to find a dentist who can best help your sleep and breathing
If the health of your airway is important to you and you want to get your sleep on fleek, then you need to check out this interview.
You can watch the interview here.
Learn more about Dr. Brian Hockel
His website: Life Dental & Orthodontics
His practice is located in Walnut Creek, CA 64598.
Bio
As a graduate of the University of California, San Francisco, School of Dentistry in 1989, Dr. Hockel is a general dentist in private practice with a focus on orthodontics that aims to prevent or treat airway problems like sleep apnea.
He aims for more permanent solutions to Airway-Friendly Smiles, going beyond the dental oral appliance approach, often having to reverse previous orthodontic treatments.
He has lectured nationally and internationally on topics of facial growth guidance, orthotropic, and airway orthodontics, and is an orthodontic instructor for the Academy of Airway and Gnathologic Orthopedics (AAGO).
He is also co-founder of the Team Airway Study Club, a co-founder and board member of the North American Association of Facial Orthotropics, and a board member of the AAGO.
Show notes
Here are links to things mentioned in the interview:
Joe Cicinelli - He is our mutual physical therapy colleague, and a dear friend.
ALF - A lightwire appliance that is often used when there is cranial dysfunction present
DNA - An appliance that aims to expand the palate in multiple directions. It's akin to the Invisalign of palatal expansion
AGGA - An appliance that is used for sagittal palate expansion
A Randomized Crossover Trial Evaluating Continuous Positive Airway Pressure Versus Mandibular Advancement Device on Health Outcomes in Veterans With Posttraumatic Stress Disorder - A neat study that positively affected PTSD symptoms by targeting sleep.
Upper Airway Resistance Syndrome Patients Have Worse Sleep Quality Compared to Mild Obstructive Sleep Apnea - If you have never heard of UARS, then this is a must-read
Bruxism: A Literature Review - An excellent in-depth article on all things bruxism, grinding, clenching, and more.
Modified Transcripts
The difference between conventional dentistry and airway dentistry
Dr. Hockel: I think a lot of it has to do with the understanding of how we get to where we are and what the underlying causes are of some of the problems that we're dealing with. And then the connections to what we're doing in the orthodontic world, the orthopedic world. By that I mean if you understand that our growth really affects our function, especially of the airway but certainly of the jaw joints and of the bite, how those relate to each other?
if someone says “we are the way we are because of our genes; we're just going to grow.” “This is a set shape to the skull, a set position for the jaws and it is what it is and make the teeth fit within that confine of the skeleton.” That's going to lead you to a very definite approach in orthodontics.
As opposed to the belief that the way we posture our mouths and the way we use the muscles of our mouth and head and neck, that's going to affect how our face grows at a young age.
Then as an adult, it's going to affect the function of the airway, again of the joints and that maybe if we look for the underlying causes and address them, we can have other successes beyond just getting the teeth to fit.
So it's looking beyond how the teeth fit together and looking at the overall structure; jaws, airway.
It turns out that the roof of the mouth is the floor of the nose. The nasal airways are our next-door neighbor that way going up and the oropharyngeal airway is right behind the tongue. We're always looking at the back of the throat but we don't recognize that that's where the air has to go to be able to breathe. So there are neighbors in the dental world and it turns out that the things we do affect them.
Zac: It's a lot more than making a pretty smile in terms of the impact that you can have on someone's health and well-being.
What kind of implications or negative things have you seen from people who don't respect that? We've spoken before having this conversation about some people who are just doing retractable orthodontics which maybe you can talk about. They're just pulling teeth so things can fit and the smile can look nice.
What are some of the implications of not taking into consideration the structure of the face?
Dr. Hockel: It might be an overstatement to say that most orthodontists are focused on just making the teeth pretty because obviously there's a lot of science that goes into how we try to make the teeth fit. Jaw joints and even airway are in the conversation, though the latter seems to be lip service.
The best way to answer your question would be to use a term that was coined by Dr. Bill Hang in Southern California, he calls it ERRS (extraction retraction regret syndrome). He purposely called it errs because it's based on the answer to your question, what are the errors that we've been forced to live with?
The first is kind of an aesthetic one where people don't like the way they look and with a lot of traditional orthodontics. There's a feeling like maybe the teeth are further back in the face than they should be or the lips seem sunken in or thin. There might be a feeling like the face has lengthened after orthodontic treatment has been done.
Then there's the whole functional side and this includes, both the airway and the jaw joints and also includes the bite, of course, the way the teeth fit together can be affected by that. How we chew and how we breathe, they can go hand in hand.
If you bring teeth too far back in the face, the tongue doesn't have enough room, the chewing motions of the jaws can be affected and of course, the dimensions of the oropharyngeal airway can be affected. People who live with this for a long time and have been told this or that thing is all in your head and you just need to learn to deal with that.
[caption id="attachment_12855" align="alignnone" width="810"]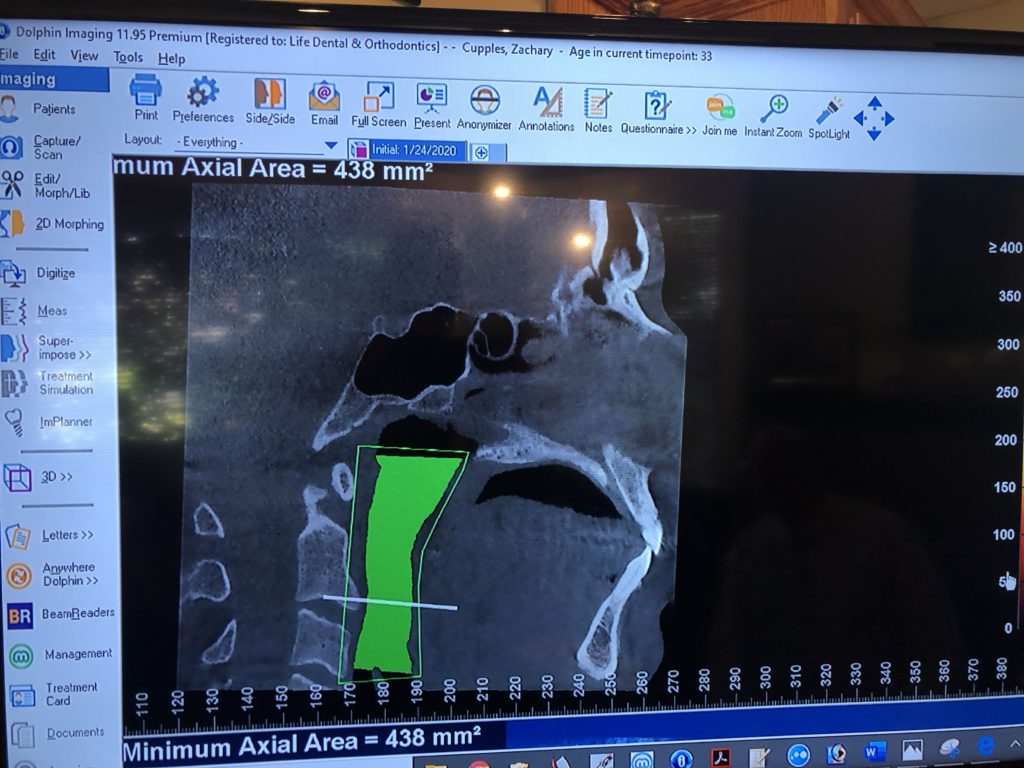 How embarassing[/caption]
How embarassing[/caption]
We who work in the orthodontic profession may be saying your bite is fine, everything fits together, it meets every possible standard that or criteria that I could have treated it to. So whatever you're not happy with, it's not what I did and maybe I did treat to the best standard of care that's out there.
But we're learning now that there are things beyond what we've been held to and by ourselves and others and what we try to achieve that have really profound and far-reaching effects that we weren't even aware of.
Zac: I mean you just think of this area of the body, you have most of your sensory systems there. There’s a lot of prime real estate that could potentially be influenced in one direction or the other.
It's intriguing that you're saying the wide-ranging effects that can happen on this. I remember a study I read years ago about people who had PTSD. They put an appliance in the person's mouth as treatment in this randomized control trial and it had a profound impact on symptoms.
We can have large substantial changes on someone's health and well-being by affecting this area of the body in the way that you're talking about.
Now you weren't always into the airway side of things so in your career what led to you appreciating this side of dentistry more?
Dr. Hockel: I think it was contact with doctors like Bill Hang and John Mew.
John Mew is an orthodontist in the UK who for many years developed treatments that were based on what he called the tropic premise. That was the belief that the jaws are going to grow to the position that they most commonly adopt, so keep your jaws closed, pointed forward they're going to grow forward. Keep them apart, pointed away from each other they're going to grow away from each other.
It turns out that the treatments he was doing to get the face to grow to what was a better proportion, more aesthetically pleasing result; it was also making a difference with the airway.
Initially, he didn't really even realize this so he's one of these people that looked at the results of what he was doing and actually saw something really good. There were a lot of us that looked at the results of what we were doing with more traditional methods and saw that we weren't doing things that were good.
Bill Hang, who I already mentioned, is probably the biggest influence on how I’ve been able to connect the dots between the airway and what we do in the orthodontic and orthopedic world.
I thought I had every answer that I needed at one point and I suppose sometimes we get that state of pride in our careers. At first it can be unnerving to learn something new but then you can get to a point where you're kind of in a zone, you feel comfortable and I felt like I had a tool to treat pretty much every type of bite problem that I could come across.
It was right then that Bill Hang dropped into my life and taught me to look at things in a very different way that included growth direction, growth guidance, developing more space for the tongue, looking at the oral posture. Especially looking at what was happening with the airway and how things affected that.
Like most of the people who've heard Bill Hang, there was some of it that I readily accepted and other things I was skeptical about. I had to go home and think “I don't know if he's really right about what he says about the herbst appliance” for example. I’m going to go home and look at my cases a little more critically and I just shook my head as he was right.
There were things going on that I didn't want to have going on right under my nose because I wasn't paying attention to it. So now my attitude is “just don't cause any harm, don't do anything that's going to make anything worse.” “And if you're doing something that has made other people worse and you're not sure if it's going to make this person in front of you worse, just don't do it,” it's the safest thing to do.
Zac: Yeah and I imagine too if you're not taking into consideration things like oral posture airway and things like that just because of how important respiration is. You could have wide-ranging effects of doing harm that you didn't know you were doing.
Dr. Hockel: Right or at least miss the opportunity to do good, to me that's just as bad; if I had an opportunity to do something a lot better for someone and I missed the chance, I don't like that.
Zac: Was that hard for you to have that kind of paradigm shift?
Dr. Hockel: Yeah my wife would tell you, I was in a very difficult mental state during those years. It was a big paradigm shift and very emotional and around that time we had a lot of little kids around the house. It’s hard to realize your professional foundation isn’t as solid as you thought it was. I knew however, that I needed to keep growing and learning; not being foolish to where I thought I knew it all.
Zac: Yeah, that's when you know you need to retire or quit.
What types of patients would benefit from airway orthodontics
Dr. Hockel: I think the people that search me out know that there are important ramifications of the types of treatment we do in orthodontics and in growth guidance. And they don't want something bad to happen to their kids or they're an adult that has already seen something that happened to themselves.
We talked about extraction retraction regret syndrome and there's either an emotional component or an aesthetic component, more often I see the functional component. People will come wanting to know what they can do to improve their situation as an adult and some of them might come very bitter about what was done with them in orthodontics.
It's unfortunate because the person who treated them was only treating what the standard of care was at that time and they probably did a very good job.
[caption id="attachment_13014" align="alignnone" width="500"] Making kids unhappy in more ways than one since 1960 (Photo credit: Orthodontist101)[/caption]
Making kids unhappy in more ways than one since 1960 (Photo credit: Orthodontist101)[/caption]
I don't see too many people who were treated by an orthodontist who did a bad job; they were just doing it with a very different philosophy of how to treat and why to treat. So there are the moms with the kids that want them to grow right, that's a group of people who have young kids and they want to catch them as early as possible.
The earlier we get to kids the better.
I’d rather get kids at six days old and talk to the parents at that point. Make sure there's no tongue tie, make sure you're breastfeeding as long as you can, try to switch to solid food as early as you can, and the whole concept of baby-led weaning. Take away bottles, pacifiers, and sippy cups.
So it's not classic orthodontics to talk to a parent about their child when they're that young. And yet, if they follow what advice I’m giving them, it can help minimize what I might have to do later on.
I think the goal would be for us to really find as far upstream as we can go to find the causes that can be addressed so that we don't have to treat them at the stage where we are. Even at age four and five when I’m treating a child that young in a way, it'd be better if I could have got them earlier.
Tongue ties
Zac: It seems like even the concept of having your child have a tongue-tie release is very controversial. I read stuff on the internet all the time where it's like “oh, we don't need to do that” and it's unfortunate because it can definitely negatively impact things like breastfeeding and things of that nature.
Let's say I have a kid and I say “Dr. Hockel, do unto this child what we can do to minimize any negative effects,” where would you start?
Dr. Hockel: Well those things that I just tossed off a little bit of a list when they handed me that little scissors to cut the umbilical cord in the delivery room for my kids. I look back on it now and think I probably should have just looked around like lifted their tongue going “okay, I’ll just do that first!
Tongue ties can affect speech and growth. When they’re really bad and a lactation consultant picks it up and says you're not able to breastfeed because of the tongue tie, they deal with it. Or if a speech pathologist says your child can't make those sounds because he's tongue-tied, they deal with it. But there's a wide range of restricted mobility of the tongue that can come before you ever have any of those kinds of troubles and it does affect the tongue posture.
There's research that's being done now by Souresh Zaghi, but it’s going to take time to build the evidence body.
They showed at Stanford that when you have a tongue tie, there's a correlation with narrow palates, and it kind of makes sense, it’s common sense. The tongue is the scaffold of the palate so if it isn't able to posture up against the palate, how is it going to grow wide and up and forward? It's going to tend to be narrow and down and back.
While we cannot expect adults who get a tongue tie release to grow differently, we do know that the muscles of the head and neck can be in better balance with good oral posture. I’m not an expert in cranial osteopathy but I’m told that the cranial bone and the balance of how they fit together and move, you know cranial bones move right?
[caption id="attachment_12694" align="aligncenter" width="329"] Now I got the loosest tongue in the game...wait....[/caption]
Now I got the loosest tongue in the game...wait....[/caption]
Zac: Haha yes I do!
Dr. Hockel: Some adults will report some wide-ranging improvements of symptoms and you got to be careful about that. Because they'll tell their story on the internet and somebody else thinks “oh if I go get my tongue-tie release, all my troubles are going to go away.”
It is controversial probably because there's such a wide range of techniques in doing it. Back in the day, I got my laser in 1999 and I thought “oh, there's a tongue-tie, I’ll just release that tongue-tie with my laser” and it's like getting a lightsaber on Star Wars. There's no bleeding and all of a sudden the tongue can just elevate really easily.
Mainly, all I was treating was that flap of tissue on the outside not knowing that there were deeper fibers that of fascia or even the mylohyoid going deeper that needed to be dealt with. Then the scar tissue would come because I wasn't having them do exercises afterward and the scar tissue ends up restricting the tongue down even more than it was before.
Doing it the wrong way is oftentimes going to make things worse and not any better at all so the data points that people have to compare to are very limited.
The unfortunate thing is we currently lack a body of knowledge out there of training. It's changing slowly because people know improvement when they feel it. You can't put an idea in somebody's head that effectively after I do this all of a sudden you're just going to imagine that you have a tension release in your whole head and neck area. They're going to tell you stuff like that or you see a child who has a tongue tie and you get a certain growth direction improvement. Then don't treat the tongue tie and you see the growth direction tend to drop back, that's kind of the lost opportunity side of it.
You want to get everything going in your favor for optimal mouth posture.
Facial underdevelopment
Zac: Now if you have someone who was breastfed, had a tongue tie release, did myofunctional therapy, addressed nasal patency, do you see a reduced need for orthodontic services down the line? Or do you think that our altered cranial shapes are generational?
Dr. Hockel: If I had seen that happen here or there, that's such a small number of patients, it's really anecdotal and there's confirmation bias. I’m not sure how valuable that would be, I do know that I see patients who were breastfed very early on and their parents follow Westin Price. They feed them really well and try to avoid sugar and stuff, they avoid bottles and pacifiers, avoid milk, avoid wheat and they seem to be doing all the right things.
Yet there are still issues there so there's so much that we don't understand about it. I feel like we're just at the tip of an iceberg and we're doing our best, we know certain things do affect it and we're trying to change those but we don't know everything.
I can sympathize with the mother who says that “I’ve done all this, what else do I need to do?” Well, sell everything you own, give it to the poor and then maybe… I don't know.
Zac: It's hard, especially in health and wellness. You want people to do everything right. They eat healthily, they're sleeping and they're doing all of this, but sometimes there are genetic factors, epigenetic factors, and exposomal factors outside of your control that are the rate-limiting steps. It's unfortunate. But life's not fair either so I get that.
Airway orthodontics for children
Dr. Hockel: Orthotropics can be used for kids in a particular age range. There’s a narrow window because orthotropics is growth guidance, and if you're trying to guide growth you need growth to be able to guide.
There are actually a couple of different windows where you can do it but for practical reasons, it tends to be a better fit somewhere in the 7-10 age range. In England, they'll say eight is too late, but in America, we tend to do it at nine or ten as well.
The older you get, the less growth there is and the less cooperation there is to be able to do what’s required for the treatment. So guiding growth and starting at that age; say seven or eight, you want to look at how the face is growing. You want to look at imaging to see how the airway might be restricted.
Although you can’t diagnose from imaging, it's a glimpse into what's going on in the nasal airway, the oropharyngeal airway, and tongue posture sometimes.
Then you look at obviously orthodontic issues like how the teeth are fitting together, and how the jaws are fitting. If the jaws have not grown as far forward as they should and there's an oral posture issue, those are two things you can consider affecting at that age.
Younger than that age, it's harder to make a change with how the jaws are growing with appliances and postural changes, and after age 11 or 12 it's very difficult, so during those middle years is prime time for treatment.
I had two boys in my office yesterday morning. Both of their faces were tending to grow more downward and backward than they should, and I always say “welcome to our world.” That's all of us to one degree or another much more so than our ancestors a few hundred years ago.
I looked at their imaging, teeth, questionnaires, and my notes from their exam and I thought I think they could really benefit from just simply widening out the dental arches. This would give their tongue and teeth more room. Then releasing the tongue tie could really help oral posture.
Then I got their sleep studies. Both boys had overnight sleep studies and had sleep apnea at over 11 events an hour. For a child that's severe. For you and me it'd be 32, 35 or 40 times an hour (normal is less than 5 per hour). When I saw that, the scale was tipped WAY in favor of orthotropics. Meaning it'd be worth the cost, the time, and the hassle if the parents and the patients were candidates for it.
Cooperation both by the child and by the family is so much a part of orthotropics. It's not like any other treatments that we do. Lack of family support, discipline, or money are all factors to consider.
What I like to do is look at what are the problems; what are this family's capabilities and desires and then what's possible from a technical point of view. How can I put all that together in a way that's going to be a win-win and get a good result?
[caption id="attachment_13015" align="alignnone" width="810"] Yeah, let's discuss airway later honey. (Image by Dimitris Vetsikas from Pixabay)[/caption]
Yeah, let's discuss airway later honey. (Image by Dimitris Vetsikas from Pixabay)[/caption]
Had it been a family that came in where the kids were climbing up and down the chairs in the room, they weren't listening to me at all when I talked to them. The mom's on her phone trying to carry on a conversation at the same time talking to the dad who doesn't live with them and is trying to tell him “don't worry, I’ll bring them over;” you know just a lot of other challenges in life for a situation like that.
Even though I knew it would make a big difference for them, I wouldn't even mention the word orthotropics because it's going to be frustrating and in the end, not a fruitful endeavor.
Airway Orthodontics for adults
Dr. Hockel: Let’s assume there’s an airway problem, have sleep-disordered breathing, and don’t want to be on a CPAP for the rest of their life. What are the options?
Although everyone is different, there are a lot of commonalities. The three general approaches are:
CPAP
[caption id="attachment_13016" align="alignnone" width="800"]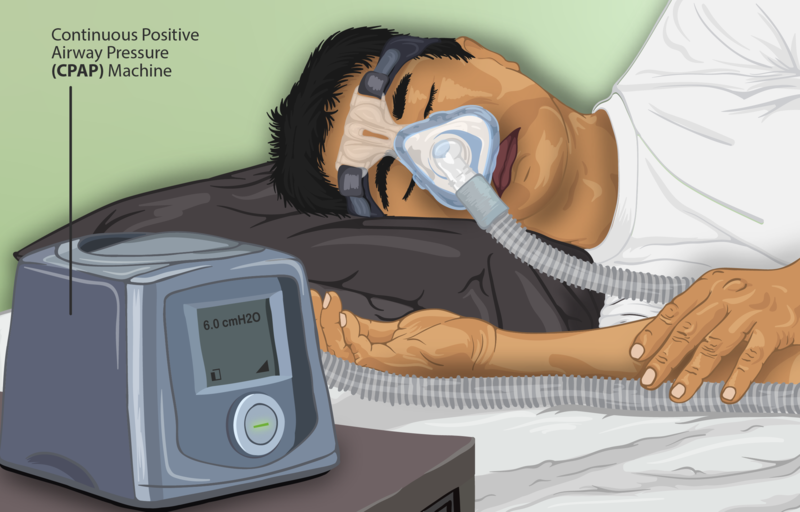 It saves lives, fam! (photo credit: myupchar)[/caption]
It saves lives, fam! (photo credit: myupchar)[/caption]
Dr. Hockel: The first is to push harder on the air going into the airway. That's the CPAP option and usually, there's kind of an x through that option, but for a lot of people, it is a realistic option. If those boys from earlier had severe sleep apnea, I told them “you need to follow the doctor's recommendation.”
CPAP is a viable first aid option. Whenever we do growth guidance, changes in the skeletal structure aren’t going to have an effect overnight, so just get some good sleep and get healthy in the meantime.
Oral appliances
Dr. Hockel: Option two would be to open the airway temporarily at night time, and that's effectively what the dental appliances do.
When you see dentists or orthodontists talking about how they treat sleep apnea, generally it's because they make appliances like this. There are over 200 different FDA approved designs for the appliances so there are lots of ways to try something and not be happy and then try something else and not be happy.
Or you get a good fit, if somebody really knows what they're doing and making these appliances, they look at other things beyond just the appliance itself then they can be effective too.
They have their place; everything has advantages and disadvantages and the big advantage of an oral appliance is you don't have to be married to this machine on the bedside table. You're not dependent on electricity, you could bring it with you when you travel a lot easier, it's less bulk in the mouth, it's not as unromantic as having this thing strapped around your head.
It’s got downsides too and that is it's not really fixing the underlying problem, it's not addressing the structural underlying problem for most people.
The other downside is that it's anchoring a lot of force, pulling the lower jaw forward on the upper teeth. So there tends to be a reciprocal effect on the upper jaw of pulling it backward and over time that can allow for changes in the bite, how the teeth fit together or even on the jaws themselves.
It may not be the end-all be-all for many years for everyone although there are people who've gone many years and have not had bite changes, but you just don't know if you're going to be that one. It helps with cardiovascular effects with sleep apnea which cpap does not.
Zac: Why is that?
Dr. Hockel: They don't know.
Zac: It is so interesting.
Dr. Hockel: It is.
Zac: Because they say CPAP will save lives right, but if you're not getting the cardio protective effects...
Dr. Hockel: When my dad heard that he said “what should I just give up on my CPAP?” I said, “no dad breathing is important, you need to be able to breathe and without that, you might stop breathing in your sleep.” “You will stop breathing and that's not a good thing,” but it's kind of artificial breathing, forcing the air in and out. And the parts of the brain that control your breathing are like “all, right don't need us anymore” and may become less responsive over time, but I don't understand the physiology of it completely. I know that it’s better than not breathing and it does save lives when it works, but the compliance goes way down after six months or so and for a lot of different reasons.
Feeling claustrophobic, drying out the airway if it's not humidifying it, restriction of movement in bed just the hassle of wearing it, the feel of it on the face, a lot of reasons why people might not want to wear it. For them, the dental appliance might be a good alternative and it's got the added bonus that it turns out it does help with the cardiovascular effect.
Zac: Is it effective in severe sleep apnea?
Dr. Hockel: It can be. Medical doctors will often tell you if you're over 30 on your AHI, the score of how severe the sleep apnea is, you should be on a CPAP. But if you're under 30, you can try an appliance.
However, my friend Pat McBride has treated more people than I know using appliances like this, including a lot of people with very severe sleep apnea, and she's been very successful at it so I think a lot of it has to do with the skill of the person making the appliance and how they adjust it.
It has to do with what else they do in addition to it: do they work on vitamin D levels? Nutrition? Overall body markers? Breathing mode? Are they lip taping? Is the nasal airway clear?
There's a lot else that can go into it; the tongue-tie for some people can make a difference, so it can be a part of a good regimen for some people, but then there's that risk of the bite changing.
Change the airway structure
Dr. Hockel: Option three is to structurally open the airway; do something so that the airway is able to be more open by changing the structure around the airway.
Ear nose and throat doctors do the same thing with different types of nasoseptal surgery or reduction of turbinates or any number of things there.
But what we do in the dental world is either move teeth to a different position to allow more room for the tongue to come forward out of the way of the airway or work with an oral surgeon who's able to move the jaws themselves into a more optimal position.
So in both of those cases, you're trying to change the underlying structure. They have the potential of being a more definitive change to the airway but they're also more involved.
Going through orthodontics takes time and going through double jaw surgery, first of all, it has to be done right and a lot of times it isn't as effective as it should be, but even when it's done right it's still an expensive and invasive procedure. Everything has pros and cons.
In our world, we ask what can we do to change the shape of the jaws? Either by moving teeth or by moving the bones of the jaws.
Zac: I appreciate you listing out those options because I want people to know that if you do have some type of sleep issue. Like I had a guy reach out to me where he's like “I got my CPAP and my numbers are good according to my doctor, I don’t need to do anything else,” it's like it depends right? If we're just looking at pure symptom management you're probably okay but if you want to fix the underlying structural issues maybe we do need to go down a different pathway.
Using oral appliances and orthodontics to improve the airway
Zac: So there are some people who would argue that they're creating bone growth with some appliances versus you're saying moving teeth. What is the underlying physiological way that an appliance like I have (Crozat) works and what is likely not happening?
Dr. Hockel: It's a good question and it's a hard one that I don't have a fully comprehensive answer to, but I’ll tell you what my thinking is on it today. Bill Hang calls it the alphabet soup appliances; we've got the AGGA, DNA, ALF, and all these different types of appliances that are out there.
Zac: And they're all three or four letters, just like in our industry!
Dr. Hockel: Right, yeah pretty much yeah so but like you say claims are being made about the growth of the jaws and I’m skeptical of that in the way they make it sound. When you move teeth, you don't just move teeth, you move the teeth and you move the bone around the teeth.
Technically, that alveolar bone is part of the upper jaw and the lower jaw. So yes you're expanding the jaw by moving the teeth, but you're not really expanding the jaw when you think about the basal bone, the roof of the mouth, the hard palate.
In a child, you can much more dramatically change the shapes of the jaws. You can apply to pull forward force with something that touches the chin and the forehead and rubber bands come forward out of the mouth and attach to that reverse pull headgear. Not like the old headgear that pulled things backward but a reverse pull headgear at the right age can bring the whole upper jaw forward; that's moving the base of the jaw.
I think the bottom line is most of the time for adults; it's not a huge order of magnitude in terms of the growth changes.
Now you're going the right direction if you keep your tongue on your palate, you push it up there and help your oral posture. Maybe you're going to slow the worsening of it.
You're going the right direction if you expand both side to side and somewhat forward with any appliance; I mean to a certain degree if someone can get it done with an appliance that's different from the one I use then great.
I think as practitioners we get better with specific appliances by using them a lot. We learn the idiosyncrasies of them and it probably makes sense for practitioners to stick with tools that they are proficient with.
But on the other hand, I think there are some tools out there that don't accomplish the same thing even though a lot of times the people who use those appliances are talking about them accomplishing the same thing. For example, I’m asked a lot of the time what about the ALF appliance?
Derrick Nordstrom developed this appliance from the Crozat, which was a lightwire appliance, just not as light of a wire as the ALF.
He wanted to develop an appliance that was cranial compatible because he was looking at what was happening with the movement of the head bones. He found that with certain adjustments of the wires in the mouth, he could help the mouth posture and encourage the mouth posture to help develop the jaws themselves. It's a way of letting the body's healing potential come out on its own to help the body do the healing from within.
As a pure mechanical tooth moving device, it's probably not as efficient. I know it's not as efficient as other appliances would be, but it's not really fair to compare the two. Because the objectives that a good ALF practitioner is going to have are cranial stability and health; likely working together with an osteopath.
They're doing very different things than somebody like I am is doing. I’m trying to accomplish larger-scale changes in either lateral arch development or forward arch development by advancing front teeth.
As for something like the anterior growth guidance appliance (AGGA), the claim is that it's stimulating the growth center of the premaxilla, that with that pressure behind the upper front of the jaw there that now the maxilla is going to grow further forward. I have yet to see either case, research or x-rays, where that kind of growth could be anything more than dental alveolar changes. A dental alveolar, meaning the teeth and the bone around them moving, and I think they're going in the right direction.
I love to see the changes in advancing the front teeth with those kinds of appliances, but my question is what do you do after that? What about the side-to-side expansion? What about the lower jaw position? There's more to it than just bringing the upper front teeth forward. I think that's a good direction to go in. Do I think it's something that's happening with the epigenetic change now and activating the bone growth genes to grow? I don't know enough to say that it's not; I’ll just say that I haven't seen the cases that have shown me the kind of bone growth that is making that kind of a claim.
It's a very different order of magnitude of change compared to what you would do with orthognathic surgery, where you may be going forward 18 millimeters and able to change the whole plane of the occlusion at the same time. The ALF crowd would say, “but that's completely destroying the cranial mechanism,” now the bones are frozen and unable to move as they should. I'm not going to say that they're wrong about that. I don't know enough to say when they are and when they aren't, the osteopaths I know will say, “Yeah they shut down for a period of time, but they work their way back to normal.
There's this inherent healing potential the body has and that it's worth it to be able to get the kinds of changes in the structural airway that you would get.
However, picking the appliance you want to use for yourself is like telling your contractor he should use a Craftsman hammer. What do you know about the appliances? The consumer really is in a worse position than we are as professionals. We're going to lectures and hearing pro other experts talk about these things, it's confusing for us to try to piece together what's really going on.
So for the consumer to be able to do that same thing and say, “well based on what this person said I want their results, so I want you to use this particular Craftsman hammer.”
On the other hand, the consumer could say, “well to me the osteopathic angle is the highest priority and I want to work with an osteopath,” and so in the hands of that practitioner, the ALF appliance might be the best thing to achieve those goals.
Zac: It's just funny because we have the same issue in the movement industry. You have these people who are in these different camps and systems, all three or four letters.
But the tools themselves are irrelevant, it just depends on what you're objectively trying to achieve.
I actually really like how you broke it up into different camps because this was one thing that I wanted to talk to you about a little bit. You have Alf, which is more cranial osteoporosis driven, you have the Crozat which I have in right now, which is more airway focused?
Dr. Hockel: Well no, the Crozat started out as something that osteopaths like to do. In my dad’s book, Orthopedic Gnathology, is the best textbook out there on the Crozat.
The idea was that it was developing the potential that was there and the growth, both for the kids and for the adults and they knew there was an effect on the airway, not to the degree we know it now. There's a whole chapter in that book on cranial osteopathy and the pictures that are in that book are used in almost every cranial osteopathic lecture that I’ve gone to because they're well done.
So the thinking by the osteopaths with Crozats was that they were also very cranial compatible. I'm not one to say how to compare Crozats versus the ALFS, but I know Derek Nordstrom's position as the very light biomimetic forces seem to be more cranial compatible. The Crozats to me having a larger body wire on them are more effective at getting transverse arch development, especially in the back in a more defined time period.
An ALF practitioner will often go much longer periods of time than we would be comfortable in the orthodontic world wanting to have someone commit to. The objectives of the end of the treatment aren't what are focused on; it's more the journey along the way. Let's do the tweaking we need to do now, see if that's getting you going in the right direction and then nine years later maybe we're still doing the same tweaking and your bite is nowhere near fitting together.
We've been looking at the symptoms and the cranial situation, it can go in a direction like that and maybe it's helping people, I'm not going to say it's not; it's just not what I do. I can't comment on it, except to say that I want to have a more defined period of time to accomplish certain objectives and in my world, I can do that. The Crozat is a common tool that I’ll use, the sagittal designed by Bill Hang has been a very effective tool, as well as different kinds of other expansion screw appliances.
They're different approaches depending on what you want to do and it's really hard to say, “I want this appliance.”
The most important thing would be to say what it is you want as a result of your treatment? People say, “Well can you use the ALF appliance to do what you want to do with that particular appliance?” I’ll say, “yeah I could use my kids watercolor brush to paint that whole wall over there too,” it's not the most efficient way to do it, give me a roller and I’ll just go like that and there it's painted. I think certain things can be done in other people's hands if that's the way they choose to do it.
How to seek better dental care
Dr. Hockel: That's a really hard question because what job do they want to have done? What's their goal?
I think if I could rephrase your question it might be “how could I help people know whether they're seeing a practitioner?” Who's going to do things that are not going in the wrong direction for the airway and sometimes for the jaw joint? Better yet, that they're going to be focused on ways that they can help improve the airway and there are other people around the country and around the world that focus on this and we all have our different approaches, but that's okay!
I think asking questions like:
“If you have a child and the front teeth seem to be a little bit ahead of the upper than they are on the lower, what would be your favorite way to try to correct that kind of a bite problem?”
I can tell you that almost all the time the solution is going to be some type of mechanics that's going to end up pulling the uppers backward to a certain degree. We'll conceptualize in our mind that the appliance we're using is bringing the whole lower jaw forward, but that's a really hard thing to do.
So dentists end up using things to pull teeth back. Back in the old days, it was headgear, now it might be the Herbst, the twin block, or the Carrier appliance, it could be the Invisalign with attachments on the side that brings the lower jaw forward. It could be class two elastics rubber bands going from the top to the bottom. There are all kinds of things: twin force bite correctors, jasper jumper. They've invented all these different things because it's the most common malocclusion, the class 2 malocclusion.
[caption id="attachment_12200" align="alignnone" width="472"]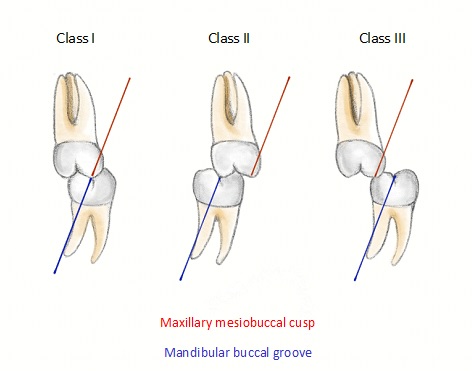 #overrated (Photo credit: Rjmedink)[/caption]
#overrated (Photo credit: Rjmedink)[/caption]
I won't say it’s where the lower is too far back and I won't say where the upper is too far forward. I’ll say where both jaws are too far back, but the lower is further too far back than the upper. So to do something that's going to pull it back even more is going further in the wrong direction, and it's not following the best principle which is do no harm.
So if you found an orthodontist that had a way of leaving those upper front teeth where they were, not pulling them back and consciously trying to hold them where they are and do something to compensate for it with the lower, you have somebody who is really on the right track.
For an adult when there's a big discrepancy between the upper and lower like that there really aren't a lot of things that they can do.
I have a patient who went to a local department head of orthodontics in the local dental school because her dentist had told her before he did porcelain veneers that she really should just get her bite fixed, which was a class II malocclusion.
They recommended that she take out two teeth on the upper and just pull the upper front teeth back to match the lower teeth, a very common way of fixing it that's been done for many years for many people around the world. It's considered the standard of care in many ways, but she felt that everything went downhill for after that: diabetes, hair falling out, she got atrial fib and more.
She remembers having dreams while her front teeth were being pulled back of choking. So she thought that this is probably affecting my airway health, my sleep, and my breathing. This is all on her own, from her own research, and she told her doctor, “you need to do a sleep study for me,” it turned out she had sleep apnea.
Then she was recommended to have laser surgery from the back of her tongue to reduce the size of her tongue. They recommended double jaw surgery to bring the jaws forward; of course, there was CPAP, which she wasn't able to tolerate.
She attributes all of this to pulling the upper teeth backward. Reversing that for her opening up that space again and eliminated the sleep apnea!
Her hair didn't grow back, but she felt overall so much better and people report little things that they notice along the way when you reverse that kind of extraction orthodontics. Our experience of patients reporting what negative things they went through, the extraction retraction, regret syndrome stuff, in her case it was functional, but it became emotional and aesthetic too. She didn't like how her face looked with those teeth further back.
People generally look better when you bring the teeth forward. Their lips look fuller; they aren't sunken behind a line between their nose and their chin.
She's a good example of an overjet problem. When people have this they have an overjet problem, but they call it overbite.
Zac: Just so people have that definition and I know this is not correct. It's when the top part the top teeth appear to be further forward than the bottom teeth even though from a facial structure standpoint that's not the case, versus an underjet, commonly misnamed an underbite would be the reverse of that where the lower teeth appear further forward than the upper teeth even though both are back.
[caption id="attachment_13017" align="aligncenter" width="255"]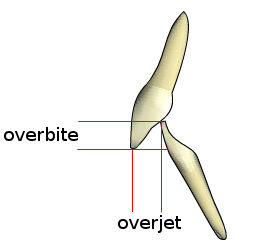 Overjet is front to back, overbite is top down (chrome spinnin') (photo credit: Nielson2000)[/caption]
Overjet is front to back, overbite is top down (chrome spinnin') (photo credit: Nielson2000)[/caption]
Dr. Hockel: Yeah exactly, even though both are back that's the key, you see people with these really big chins, they're probably too far back.
Zac: Like Jay Leno?
Dr. Hockel: Like Jay Leno, his chin is actually not too far forward, if you put an outline on his face and make a comparison to the ideal. You'd see that it's really mainly the upper jaw that needs to be more forward and his lower if anything is slightly back.
[caption id="attachment_13018" align="aligncenter" width="272"] HE HAS AN UNDERDEVELOPED JAW?!?!?!?! (photo credit: Wikimedia Commons)[/caption]
HE HAS AN UNDERDEVELOPED JAW?!?!?!?! (photo credit: Wikimedia Commons)[/caption]
Zac: Gosh could you imagine if he worked with you, he would have the most prominent chin.
Dr. Hockel: No he'd have a balanced face because we get the whole midface further forward. He probably has sleep apnea as a result because his tongue must have nowhere to go. You see in his smile, it's a very narrow upper arch. Poor celebrities getting diagnosed by us dentists all the time on TV.
Another thing to ask a practitioner is:
Do they think that there are times when it's worth taking teeth out and pulling front teeth backward? Are there cases they think that can be helpful for?
If they say yes, I would probably just go somewhere else because if it's okay for an exception it's probably okay as a general rule. I'll tell you, the last time I took a tooth out and pulled things back it was when somebody had five lower incisors.
Zac: Normally there are four.
Dr. Hockel: There are four, so taking one out and pulling them together now we're just right back to where a normal set of teeth would be. Although there's a case to be made for leaving that tooth in there, allowing the lower arch to be that much bigger and then just making the upper fit bigger over the top of it. That would be a question to ask you:
How do they know if there's an airway problem?
If your medical doctor has told you have sleep apnea then I know you have an airway problem and you might want to ask:
Is sleep apnea the only kind of breathing disorder that you address? What are the ways that you address it?
If they say yes, that's the main kind of disorder we treat and we treat it using appliances that bring your lower jaw forward. Well on the diagnostic side, if sleep apnea is the main thing that's being treated they might be missing something that's even more prevalent than sleep apnea and that's upper airway resistance. It's a whole side to sleep breathing disorders that get missed for kids, for thin, fit adults; people like you or women especially. It isn't always apneas, although the sleep medical doctor I was talking to yesterday was telling me if you score the sleep study the right way you'll see the apnea is there.
It's just not things that would be traditionally called an apnea, so finding upper airway resistance as a potential confounding factor of these patients who have problems is important.
I think for the dental practitioner either working with a medical doctor who knows what they're doing with this or maybe helping the patient get the sleep study yourself.
Another important question to ask would be:
If they are finding the upper airway resistance, then what are the ways that you try to treat it? Are they doing expansion arch development, getting the tongue more room, and working with a myofunctional therapist, in either their office or somewhere else to try to optimize the oral posture?
If that's not a part of what they do to try to treat it then they're probably not as deep into this rabbit hole as they should be, because that's at the outer rim of the rabbit hole. That’s the basics: create more room for the tongue however you're going to do it, don't close spaces generalized.
You could ask them:
If my child has a lot of gaps between his teeth, how would you tend to treat that? And whether you do it with Invisalign or braces or whatever to take spacing between teeth and close all that spacing up?
You're talking about a friend who had a bunch of missing teeth, when people have missing teeth the jaws don't develop to the size they should. If you just close all the spacing where there were teeth missing the tongue is going to have much less room to fit into, it's going to go back toward the airway and there's going to be a risk for sleep apnea, so that's another combo.
Zac: The big things are you want are:
- Moving teeth forward and outward
- Prioritizes expansion
- Appreciation of sleep disorders
- Focus on attaining palatal tongue posture and adequate lip posture
- Utilizes myofunctional therapy
Dr. Hockel: Yeah it's the tongue posture and the lip posture: lips together at rest all the time breathing through the nose and the teeth either together or in near contact. so lips together, teeth together, and tongue to the roof of the mouth; those are the three things posturally that a good myofunctional therapist is going to work towards.
Keeping Our Wisdom Teeth
Zac: Now I want to talk a little bit about getting teeth pulled, the ones that I'm going to bring up of course are the ones that are old remnants from caveman days, wisdom teeth. I was recommended by a practitioner to get mine pulled out, I didn't get them pulled out when I was 18, I actually pulled them out in my late 20s. The reason why I got mine pulled out was because I had no lateral jaw movement. Are there instances in which you should have wisdom teeth pulled out?
Dr. Hockel: In the ideal world we would not have to take wisdom teeth out. In the ideal world, our jaws would be further forward and we would all look way better than we look now. In the ideal world, our airways would be massively open, we’d be breathing through our nose, and our muscles would be much stronger to support that.
We're not in an ideal world, so taking wisdom teeth out now it’s not the best way to go, and our hope in developing more forward growth of the jaws is that there would be room for them, but sometimes there just isn't room for them. Sometimes they're at crazy angles and you really don't have much of a choice.
I don't tend to focus too much on the wisdom tooth issue. As much as I’d like everyone to have 32 teeth in position with the way they should, once the growth is done (age 12-14), there’s not as much that can be done to make a difference in how much room they have or whether they come in.
In my family, my dad tended to have us just keep them in our mouth and he didn't want to take the wisdom teeth out. So I still have all four of mine, I’ve got all 32 teeth and occlusion, but it's still somewhat tight on space back there.
I think it's the case that when you leave them in you tend to get more growth of the jaw. I can't prove this and I don't know if there's research to show this.
I’ve had a lot of kids where they'll come in and maybe the general dentist has said take the wisdom teeth out I'm looking at them thinking, “you know what there might be room. You're only 18, go another seven years let's see how you grow.”
I think that there's more and better jaw growth as a result of those wisdom teeth being there. We know that people like your friend with missing teeth get less jaw growth; why wouldn't having extra teeth back there help encourage more jaw growth?
At the same time, as an adult, if you're wisdom teeth are sideways pointing forward, now it's a liability for the bone integrity around the back of that molar in front of it better not to take that chance.
I know that there's a discussion of meridians attached to different teeth and I'm not an expert in that. People might tell you if you lose that tooth that's going to affect some other part of the body, that may be true, but I'm just not sure what the best compromise is. I’d rather not lose that second molar in front of it by having more bone loss there, and I’d rather just lose the wisdom tooth.
Zac: Yeah because I think in my case, mine were pointing straight forward at least on the lowers.
Dr. Hockel: There probably was nothing that could be done to try to straighten them yeah and even if you went and did heroic orthodontics to try to move them up then where are they going to go? There's no space back there.
Occlusion
Zac: When I was first getting exposed to this even being a thing because in PT school, we never talked about when you need to refer to sleep apnea or how teeth influence things or anything. My anatomy is still lackluster up here; what is occlusion? Is it from your perspective an important thing that we need to consider? I know that they make appliances to alter occlusion, if you could just give a little overview of that I think that would be amazing.
Dr. Hockel: Sure, that's kind of where I started, I was a senior in high school and my dad said “I bet you could earn more making teeth than you could slicing salami at the deli where you're working, why don't you give it a try?” I was like sure, I don't know what it really involves but that was my start in dentistry. I was working as a dental technician doing full mouth reconstruction. We call it wax up where you create and wax how the teeth should fit together, upper and lower, and it's a very precise scheme of how the teeth should fit.
Gnathology was where I came from and people who are in dentistry would know they're kind of different camps of different types of occlusions and gnathology is the one that really raised the bar for how teeth should fit together.
There were certain principles you always tried to follow with it, and as a dental technician and as an early years in practice as a dentist, I focused a lot on the occlusion of my patients and trying to get the bite right.
Gnathology means trying to get the bite right, but it turns out that some of the things we do to try to get the bite to fit right can work against the bigger picture. So I’m not against looking at how the occlusion fits and trying to be as precise with it as you can, but that's a tree. And if you don't see the forest, then you're way down a side path that's going to be very distracting.
We'd always try to get the canines to touch each other to guide the jaw as it moves side to side. It's called canine guidance, and the thinking is that there's enough leverage this far forward in the jaw to separate the back teeth as the muscles are chewing side to side.
It's got leverage against the muscles way back here if the molars right next to the muscles that are chewing are the ones that are mainly hitting when you go side to side, it's much stronger bite forces and it's a risk for wear or for the fracturing of the teeth.
The idea was the front teeth protect the back teeth and the back teeth protect the front teeth; when you close, the back teeth should touch stopping the closing motion of the jaw. When you move side to side, the front teeth should touch so that you can bite through things and so that you separate the back teeth in those other positions.
All this works great if you have jaws in a face that's in the right position so that now the joint is in a favorable condition and the airway is in a favorable condition.
If you have jaws that are somewhat too far back, take the case of my patient who had the bicuspids extracted and the front teeth pulled back. They did that partly because it looks better but mostly because we're just taught that's how teeth should fit together; the front teeth should fit with overbite and overjet. Also close contact or maybe slightly away so that they can slide against each other to separate the back teeth during the chewing movements.
The problem is her jaws were already too far back and by pulling front teeth backward to meet against the lowers for the sake of what we disclusion, the best functioning of the teeth against each other. It can be making things worse for the airway, it can also be making things worse for the jaw joint when front teeth are brought back so that you have that contact which in the gnathological occlusal philosophy you want to have. Then it can tend to cramp the style of the joint, the whole lower jaw can be held in a position that's too far back.
That was one of the things in the early years of learning about the airway is how do I mix this with my occlusion...I won't say beliefs, but it's almost like beliefs. There's no research to show that this kind of occlusion is better than that kind of occlusion. Even class one, ever since Edward Angle the father of modern orthodontics came up with his ways of putting a bite together and one of them is the molars need to fit like this what we call class one.
There's no research to show that that's any better functionally or any other way than any other kind of occlusion. So yeah I had to balance how do I mix gnathology with the airway, and I think that you always put the airway first.
Michael Gelb has termed this ‘airway centric;’ instead of having a centric relation which is what his dad and my dad and I would all be worried about. How do you make the teeth fit together when the jaws are in their center position? That would be the best connection of the two. The tooth home is the same as the bone home and they just work in coordination with each other.
Well, maybe the bone home is pathologic, maybe there's something about that bone home that isn't right. Because maybe the lower jaw and maybe the upper jaw belongs further forward for the sake of the airway or for the sake of the function of the joint if the little disc gets displaced, then the lower jaw might need to be further forward.
If we do things with the bite, the occlusion, that works against that, the results are never going to be what they should be.
Another philosophy of occlusion might be to go to where the muscles in there are in their most relaxed or harmonious state and make the teeth fit there. Here again, in any philosophy of occlusion, if you're not looking at the airway function, you might be going down the wrong path.
Zac: It's funny you mentioned Michael Gelb because that was the first appliance that I was exposed to. I wore it because we were trying to improve my jaw motion, and I definitely got some interesting changes within my body.
Dr. Hockel: His dad Harold Gelb is the one who developed the appliance. It allows the bite to open and it allows you a lot of times to bring the lower jaw forward a little bit, which can decompress the joints. It can be good for a TMJ appliance and without knowing it, it was sometimes also helping the airway.
Zac: Yeah, but it's also doing so without necessarily affecting the airway dimensions or the health of the airway, whereas it may be affecting other areas like you said the TMJ.
Dr. Hockel: There are some people that when you put a thickness between the teeth, the lower jaw rotates as the lower jaw opens, it goes backward. There are some people that put a thickness between their teeth like that and it can make the airway worse, it'll make them grind their teeth even more so it isn't the same for everyone.
Zac: Interesting, because they definitely said it would be bringing my jaw down and forward.
An analogy in my domain is shoe orthotics. Sometimes, shoewear is something that we can use to influence someone's movement versus not. I’ve had people where we've put them in really supportive shoes and have a completely undesirable outcome from a movement perspective versus someone having those same shoes doing very well. It's just funny how you kind of have the same thing.
Dr. Hockel: We call them the same thing; you call it an orthotic, we call it an orthotic.
Dental pathology.
Zac: There are a lot of other pathological processes that some people may be dealing with. Like people who have gum recession or crowns or veneers; I don't know much about this. Sometimes I’m sure that my clients and people are getting exposed to these things, how does that influence and play a role in the airway health?
Tooth implants
Dr. Hockel: Well you didn't mention implants. If somebody's thinking about getting an implant, but they also think they may have bite or jaw position or airway problems, they've got to be analyzed and diagnosed really completely first from the big picture before putting in an implant. Because once an implant's in, it's not going to move ever; it's just going to stay right where it is.
I’ve had patients where I’ve had to do a lot of expansion of the arches and just leave the implant where it was. So in the end, the implants are like way over here toward the inside and sometimes you can work with it and just kind of warp a tooth out to where everything else is and leave it.
But I’ve had other people where the implant has to be taken out and then put back in or another crazy way I’ve done it before is to have an oral surgeon just create corticotomies. Cut around the bone where the implant is and then I’ll make an appliance so that after I’ve expanded everything else, he just cuts the bone around that section where the implant's sitting and then moves it out into the position where it belongs. Then we just let the bone heal there.
Don't do an implant until you know where it's going to need to end up. I saw someone yesterday that's going to need one for an upper front tooth and their front teeth may need to be in a different position. I’d rather catch them now and say just don't do anything until it's in the right place.
Gum recession
Recession is the gums moving down the root of the tooth exposing some of the roots, and it's generally a function of some bone loss around the tooth as well. It's not a good thing, but you don't look at any gravestone and see recession as a cause of death, it's usually not even a cause of death of an individual tooth even when there's a lot of recession. It's the bone between the teeth that tends to hold the teeth in really well so it's not a crazy bad thing if somebody does have some recession.
Having said that, you'd rather not have recession. So we look now at ways of expanding the upper jaw for example, that the base of the upper jaw will expand skeletally so that the teeth don't have to be moved in a way that might risk recession.
Of course, there are procedures the periodontists can do to help minimize it or add bone back to those areas, different kinds of bone grafting procedures. It's sometimes a necessary evil.
But it's often a sign that something's going wrong functionally with the tongue and the tongue space. You'll see people whose teeth don't even meet together in the front and they have recession. It's not from heavy bite forces or clenching or grinding on the teeth that caused it which is one cause of recession; it's like if you take a fence post and shakes it, the dirt kind of moves away and you're going to lose the support down where it's coming out of the ground.
If the bite is putting forces on the teeth up where it comes out of the ground at the gum line, the bone may be getting lost and the gums may be receding. That would be like shaking the fence post but in the analogy another thing that happens you get a cow that comes up to the fence post and just leans against it all day long. That can also make it come loose and lose the support down below.
That's the tongue on the inside without enough room putting constant force against teeth either forward toward the front teeth, sideways toward the back teeth and sometimes recession is the tongue's fault and the tongue just not having enough room.
We've been talking about the airway and when you don't have enough room for the tongue, you often want to make more room for the tongue so that the airway can be healthy. But making more room for the tongue might be important to try to prevent further recession when there's already been recession.
Zac: Have you ever seen a case where you improve tongue positioning and you give the tongue enough shape where you've had a positive change in gum recession? Because I think with Wolf's law you might be able to get some bony adaptation.
Dr. Hockel: No I can't. What I have seen is sometimes if there's a little recession in the front and you bring front teeth forward, it just from the way that it's moving through the tissue, the recession seems to look a little bit better. Other times the recession just follows it along; I don't know if there's really a pattern to when you're going to keep it or see it get worse.
For some people it will get a little worse, it's a risk of any orthodontics you could have some recession, but grafting is a possibility and trying to do things that avoid that. Moving slowly, lighter forces, and getting the tongue in balance too; get the tongue enough room so it's not going to be putting pressure on the teeth as well.
Crowns and veneers
Dr. Hockel: Those are the world of restorative dentistry and that was my world for most of the early years of my practice. I love doing crowns, I love doing veneers, I love changing the way people look with veneers and especially having been a dental technician.
I love the aspects of what makes a crown really good but it's a different world than what we're doing with the treatments in orthodontics, orthopedics, orthotropics, and airway growth, orthognathic surgery.
If those kinds of restorations for teeth are necessary from a functional standpoint, it's better to do those after you're done moving teeth around. If they're necessary for front teeth from an aesthetic standpoint, it's better to do it after you've dealt with the airway.
I had a case, his name was Jim. We'd pour some veneers for all his upper front teeth and it looked beautiful. Within the next few years, he must have broken every single one of them, just kind of grinding them off; either made them pop off or more likely just chip the corners of them.
I redid a few of them, but at the time I didn't know what was going on. I know now for sure that he had sleep apnea, there were other signs that were there. I know that it was my failure to recognize an underlying airway occlusion and functional problem.
Veneers are great but don't build them on teeth that are in the wrong place. Don't build them on occlusions that aren't functioning in the right way or there's going to be a lot of trouble later on.
Clenching and Grinding
Zac: Well I think they're actually like with… because you mentioned like clenching and grinding that's considered with some of the research I’ve looked at as sleep disorder. I’m assuming it's a symptom of something like sleep apnea or UARS.
Dr. Hockel: It's not a hundred percent but I feel like it's guilty until proven innocent; when somebody is coming in and they're grinding their teeth and they have a scalloped tongue which means indents on the side of the tongue. Meaning the tongue is a six-foot tiger in a three-foot cage trying to push out and get more room and let's say they told me they snore at night time. Now I could get rich if I could just bet the clenching and grinding the scalloped tongue and the snoring, I’m sure they've got sleep apnea. It's just a question of how severe?
But you get the people who don't snore at all and there's a woman on my practice, her name's Corey and she's got a lot of wear on her teeth, tons of wear but she doesn't snore. For the life of me I can't get her to get a sleep study because she doesn't think that there's a problem with the airway, but like I said probably guilty until proven innocent.
Most of the time that reaction of clenching and grinding of teeth is from the sympathetic reaction to the airway starting to close off a little bit, upper airway resistance, or closing off all the way because of the apnea. One of the things we can notice; scalloped tongue, a lot of wear on the teeth, recession, broken teeth, clenching, grinding; those are things that any dentist or dental hygienist can look for and see them as red flags.
Then ask the question: do you get to sleep well? Do you stay asleep well? Do you wake up feeling rested? If it's no to any of those, dig deeper and find out.
The second question is do you snore? Has anybody told you that you snore? And if the answer is yes to those two and you're seeing those other structural clinical signs, the odds are it's going to be worth doing a sleep study to find out what's really going on.
Sum up
- Airway is the most important factor when it comes to dentistry done well
- Focus should be on making room for the tongue by expanding the teeth and face, ideally at the youngest age possible
- Cosmetic dentistry should be done after the airway has been maximized.
